Indexed In
- Open J Gate
- Academic Keys
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- Publons
- Euro Pub
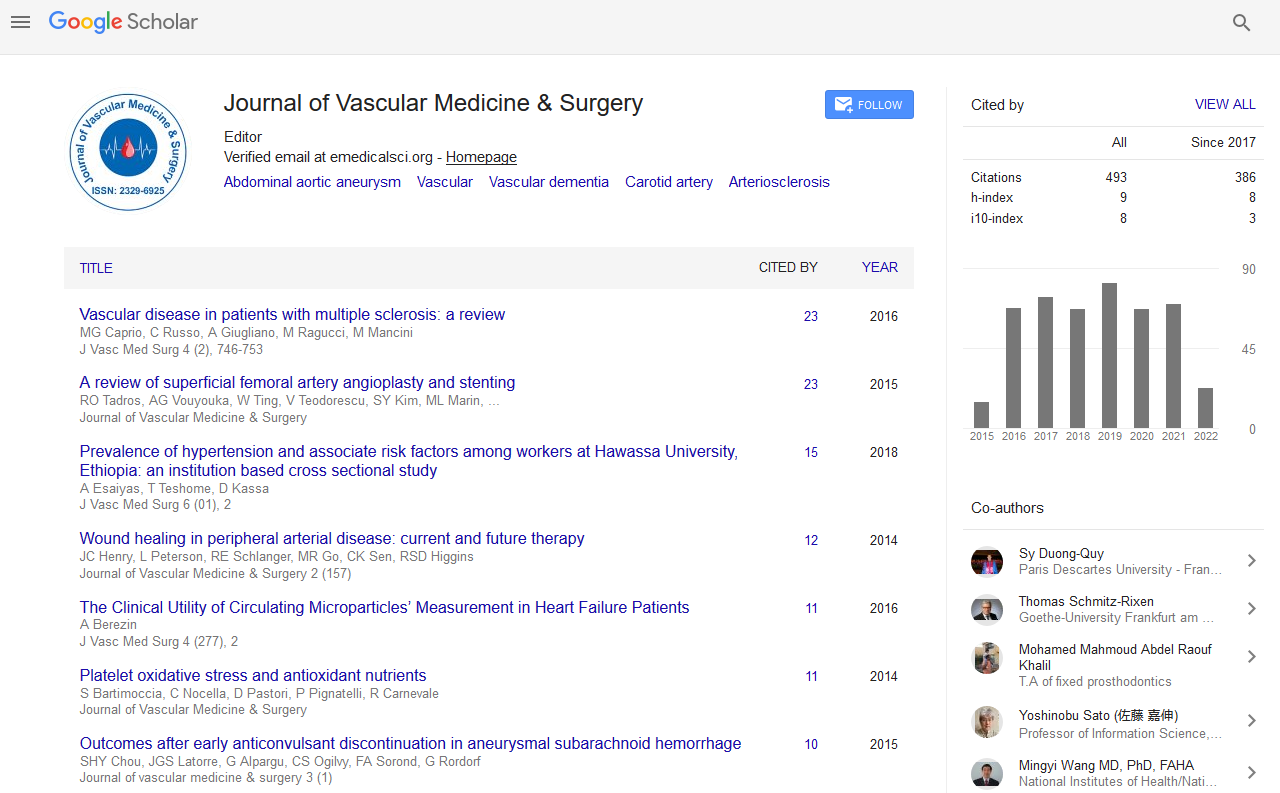
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Management of Groin Pseudoaneurysms: Indications and Outcomes for Thrombin Injection vs. Surgical Treatment
Marco Horn, Stahlberg E, Goltz JP, Rodd C, Ellebrecht D, Keck T and Kleemann M
Objectives: Persistent pseudoaneurysm of the groin is a complication related to arterial puncture following invasive diagnostic and interventional procedures. This study reports our single center results for both surgical treatment and thrombin injection (TI). Materials and Methods: In the period between January 2006 and December 2014, we analysed those patients who underwent invasive treatment for infra-inguinal pseudoaneurysm at our University Hospital. Patients for whom com-pression therapy had proven unsuccessful or was contraindicated were referred for invasive treatment. Patients with ruptured pseudoaneurysm and haemodynamic instability or infected pseudoaneurysm were treated surgically and therefore excluded from this analysis. Results: A total of 105 patients with pseudoaneurysm were identified. The mean age of all patients (50 male, 55 female) was 72.1 ([SD] ± 11.5 years. At the time of puncture, most patients (95.3%) were taking either antiplatelet or anticoagulant medication. 57 of the 105 patients were treated by thrombin injection. The other 48 patients underwent surgical repair. Indications for surgical treatment were; large hematomata with neurological symptoms, vein compres-sion or severe pain. Thrombin injection shows a high success rate of 91.2%. The majority of patients (96.5%) required only one attempt of TI for aneurysm closure. Two embolic events occurred following TI and needed surgical revision. Overall complication rate of thrombin injection was 8.8%. Surgical repair was successful in every patient but associated with high complication rates compared to TI (33.3%, p=0.003). The mean pseudoaneurysm diameter for patients who underwent surgery was larger compared to those who were treated with TI (surgery=64.4 mm SD ± 40.7, TI=34.9 mm SD ± 15.8 mm, p=0.001). Conclusions: Thrombin injection is less invasive, results in lower complication rates and reduced hospital stay compared to open surgical repair of pseudoaneurysms. Nevertheless there is still indication for surgical treatment in symptomatic and large pseudoaneurysms.