Parent-Child Interaction Therapy: Case Study of Application to a Parentally Bereaved Child
Received: 04-May-2016 / Accepted Date: 17-May-2016 / Published Date: 24-May-2016 DOI: 10.4172/2375-4494.1000293
Abstract
Parent-Child Interaction Therapy (PCIT) is an empirically supported therapy used to treat young children with behavior problems. The literature on parentally bereaved children indicates that they are at an increased risk for behavior problems and psychopathology. There is minimal literature to describe the efficacy of current intervention programs in reducing this risk for children under the age of 6 years. PCIT is designed to improve the quality of the parent child relationship and increase the parents’ use of effective discipline; two factors which are strongly correlated with decreased risk for psychopathology. This article presents a case study describing the use of PCIT with a parentally bereaved preschool child experiencing behavioral problems and symptoms of depression. At the end of treatment the child’s behavior had significantly improved and symptoms of depression were no longer observed. These findings suggest that PCIT may be an effective therapy for reducing the risk of behavior problems and psychopathology in young children.
Keywords: Therapy; Child; Behaviors; Anxiety; Autism
Introduction
Parent Child Interactional Therapy (PCIT) is an empirically supported treatment for children with oppositional defiant disorder and disruptive behaviors [1-6]. Additional applications of this therapy continue to be explored and include addressing behavioral problems in children with autism, separation anxiety disorder, externalizing behaviors like impulsivity and hyperactivity in children with ADHD, and children who have been exposed to trauma, domestic violence and child abuse [4,7-12].
Death of a parent is one of the most traumatic events that can occur in childhood [13,14] and can be extremely disruptive to a young child’s sense of security, emotional well-being and development [15]. Stability of the child-caregiver relationship is critical in helping young children develop confidence and self-esteem, learn to tolerate distress and separation, and develop self-regulation skills [16-18]. Following the death of a parent the child not only experiences separation and disrupted attachment with the deceased parent, but often with surviving parent as well, because the surviving parent’s own grief and mourning may diminish his or her ability to provide a secure and supportive environment for the child [19].
Prior research has found that parentally bereaved children frequently experience a cascade of stressful life events following the death of a parent (e.g. parental distress, moving, separation from family members, financial distress, introduction of a step parent) [20,21]. Research has found that death of a parent places a child at significantly increased risk for maladjustment and mental health problems [22,23]. These mental health problems included depression, anxiety, lower self-esteem and school problems. Behaviorally children exhibited internalizing symptoms (e.g. sadness, depression, social withdrawal, and separation anxiety) and externalizing behaviors (e.g. aggression, tantrums and delinquent behaviors). Externalizing behaviors were more frequent in boys [23-25]. Research has also found that children younger than 8 years at the time of parental death are at higher risk for maladjustment and psychopathology; possibly because of their developmental level, limited understanding of the concept of death, and limited ability to verbally express their emotions [14,23,26-28].
The transitional events model is a theoretical framework used for understanding children’s adaptation to major stressful life events. The transitional events model proposes that a child’s adjustment after a traumatic event, like the death of a parent, is mediated by an interplay between stressful life events and the child’s protective resources [29]. This model has been identified as a useful framework for designing interventions for parentally bereaved children [24]. According to the transitional events model, effective interventions would decrease a child’s exposure to stressful events while strengthening the child’s protective factors [30].
Protective factors against developing mental health problems identified the literature included, increased child self-esteem, increased internal locus of control, positive parent-child relationship, improved parent-child communication, increased positive family interactions, reduced parent distress and use of effective discipline [22,24,31,32]. Many of these protective factors are addressed in a positive parenting approach which involves creating a safe, and nurturing environment, using effective discipline, and having realistic expectations [33]. Positive parenting has been widely identified in the resilience literature as an important factor associated with positive outcomes and reduced child mental health problems [34]. Previous studies have also found that positive parenting is the single most effective protective factor associated with adjustment in parentally bereaved children [25,34,35].
Currently there is a research practice gap regarding effective interventions for parentally bereaved children [36,37]. Current empirically supported interventions are usually provided in group settings, and focus on using cognitive behavioral techniques to normalize the grief process, and facilitate adaptation to the loss of a parent [24,25,38,39]. Children under the age of 6 years present a particular challenge to using group based interventions that primarily use education because of their developmental level, limited verbal abilities, and limited understanding of death [14,23].
PCIT has not been examined for use with parentally children but is an evidenced based intervention that has been supported as effective for children with many types of behavioral and emotional problems [2,4,5,7,40]. Theoretically PCIT is grounded in attachment and social learning theory and is focused on improving the quality of the parentchild relationship and teaching parents to provide effective discipline. As a result, the child feels more safe, calm and secure, has fewer negative behaviors and engages in more pro social behaviors. PCIT outcomes include increasing parental warmth and responsiveness, increasing a child’s self-esteem and teaching parents effective discipline techniques [4]; which are specific child protective factors against maladjustment identified in the child bereavement literature [34].
Since young children cannot completely comprehend or understand the loss of their parent and have limited verbal abilities to express their feelings they may frequently exhibit externalizing behaviors in response to grief [14,23]. Instead of focusing on understanding grief, PCIT targets strengthening the parent-child relationship and teaching effective discipline techniques. The purpose of this article is to explore the application of PCIT as an effective intervention with a parentally bereaved child, through a case study presentation.
Method
Patient presentation
Jackson is a five year old boy who presented initially in the child psychology clinic for concern about behavior and school problems. Jackson’s mother died, two years earlier, when he was three years old. He is currently living with his father and his new step-mother. His father’s job requires him to work long hours and he travels for work on many weekends. Jackson is cared for by his step-mother when his father is away. Since Jackson’s mother’s death two years ago, he has moved three times and attended several different daycare centers. Behavioral concerns reported by the family included getting frustrated easily, not listening to adults (both at home and school), needing to have directions repeated several times before he complies, and being oppositional with adults other than his father, especially his stepmother and grandparents.
Jackson is now attending a kindergarten program at the local elementary school daily. He can do homework when seated with his father, but refuses to do academic work at school or for other adults. Teachers report at school Jackson chooses to follow and model children with more disruptive behaviors. Jackson’s father is concerned about Jackson’s self-esteem and confidence. Jackson had not been previously diagnosed with any developmental delays or psychiatric disorder, although there was a family history of Attention Deficit Hyperactivity Disorder (ADHD). Medically Jackson was the product of an uncomplicated pregnancy and a full term birth. He had pressure equalization tube placement for recurrent ear infections but was otherwise healthy.
Prior to starting PCIT, an evaluation was conducted by the child psychologist supervising the PCIT clinic. Observation during this evaluation showed Jackson was initially a quiet and shy little boy who kept is eyes down when spoken to. As the evaluation went on he warmed up and became more engaged when talking about playing TBall. He did not clean up the toys when told to do so by his father. In this one on one setting, he was attentive and cooperative and able to sit through an hour of testing without a break. He had clear speech and articulation and his language skills were adequate for conversation. The Achenbach et al. [41] Child Behavior Checklist for Preschool Children (CBCL/TRF) was administered to Jackson’s father, stepmother and teacher to assess his behaviors. Clinically significant T scores (at or above 70) were reported by Jackson’s father for withdrawn
(T=70) and attention problems (T=70); step-mother reported anxious/ depressed (T=74); and his teacher reported anxious/depressed (T=70), Attention Problems (T=76) and aggressive behavior (T=76). These ratings suggest that attention is a problem for both parents and teachers while aggressive behaviors and anxious/depressed behaviors are noted by the teacher and to be step mother only.
Setting
Jackson, his father, and step mother participated in nine weekly one hour PCIT sessions. PCIT was conducted in a university based child psychology clinic by a child psychologist certified as a PCIT therapist and trainer, an intern in clinical psychology and a psychiatric advanced practice nurse training under the psychologist. The rooms used for therapy were equipped with two one-way mirrors. A middle room was used as the playroom, with an adjacent room for the therapist to observe the child and parent during play. Another adjacent time-out room was connected to the play room and allowed the parent and therapist to observe the child in the time out room.
Measures
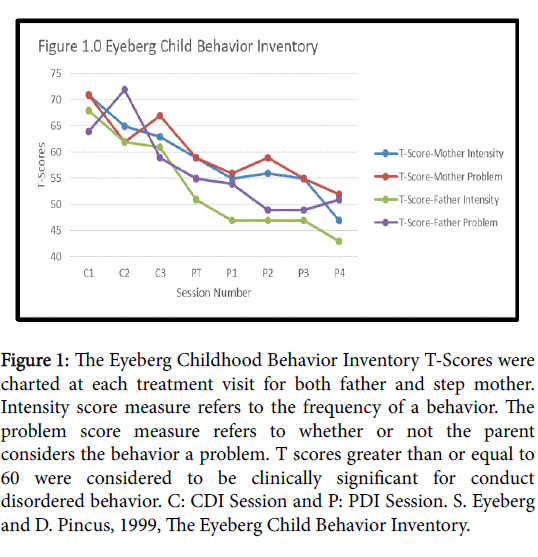
The Eyeberg Child Behavior Inventory (ECBI) [42] is a validated measure that assesses child behavior problems with two subscales; the intensity and problem subscales. Intensity subscale refers to how often a problem behavior occurs and the problem subscale refers to whether or not the parent considers that particular behavior a problem. The scale has 36 items and each item is assessed for intensity on a Likert scale from 0-7 and problem is assessed as either yes or no. T scores are generated for both problem and intensity. T scores of 60 or greater are considered to meet the cut-off for significance. The Dyadic Parent- Child Interaction Coding System Fourth Edition (DPICS-IV) [43] is a behavioral coding system designed to assess the quality of parent-child social interactions during treatment. The DPICS categories serve as markers regarding the quality of the parent child relationship. The DPICS establishes mastery criteria for Child Directed Interaction (CDI) or do skills as ten, behavioral descriptions, ten reflections, and ten labeled praises and less than three (don’t skills), questions, negative
talk, and commands during the five minute coding period.
Procedure
PCIT was conducted using the most current protocol, the 2011 Parent-Child Interaction Therapy Protocol [44] In accordance with the 2011 protocol, therapy was conducted in two distinct phases: Child Directed Interaction (CDI) and Parent Directed Interaction or (PDI). For each phase of treatment the parents attended a one-hour didactic session, followed by weekly one hour coaching sessions with the parents and child. Between sessions, parents were each asked to practice their skills during a special play time at home for five to ten minutes each day.
During the CDI phase of treatment the parents were taught to apply differential social attention, avoid questions, criticism and commands, and avoid attempting to control the interaction by allowing Jackson to lead the play. Jackson’s parents were taught to use the PRIDE sills during special play time to reinforce Jackson’s appropriate or desired behaviors. These specific skills are (P) labeled praise for appropriate behavior, (R) reflection for appropriate talk, (I) imitation of appropriate play or behavior, (D) description of appropriate play or behavior, and (E) showing enthusiasm and enjoyment. Jackson’s parents were also taught to ignore negative behaviors that are annoying, like whining, and to stop the play for aggressive or potentially dangerous behaviors [44]. During the one-hour hour weekly therapy sessions, Jackson’s parents practiced the skills with Jackson while a therapist coached them with a bug in the ear device from a separate room.
During CDI Jackson’s parents were coded using the DPICS-IV criteria for five minutes at the beginning of each session to evaluate their skills. Mastery of the PRIDE skills was required before parents could move to the second phase of treatment which is PDI. Mastery was achieved when both parents were able to provide ten labeled praises, ten reflections, and ten behavior descriptions with no more than three commands, questions, or negative statements within the five minute coding period.
During PDI the second phase of treatment, Jackson’s parents learned to give clear direct commands and labeled praise for compliance and how to use time-out for noncompliance. A specific time-out procedure was taught and initiated when Jackson disobeyed a command given by his parent and did not end until he obeyed the command. In between the commands Jackson’s parents continued to use the PRIDE skills learned during CDI to reinforce desired behaviors and nurture the parent-child relationship. During PDI sessions the therapist used the bug in ear device to coach the parent regarding their use of the skills, encourage the parent and provide emotional support during stressful times of noncompliance. Jackson’s parents continued to practice both CDI and PDI skills at home during five to ten minutes of special play time daily. As Jackson’s parents become more confident they began using commands and PDI techniques at home outside special play time.
During PDI, both CDI and PDI, skills are each coded for 5 minutes using the DPICS-IV criteria. CDI skills continued to be coded during PDI to ensure that Jackson’s parent maintained a mastery level of these skills. Mastery was achieved for PDI skills when 75% of Jackson’s parents’ commands were effective within the 5 minute coding period (i.e. when Jackson was compliant a labeled praise was immediately and enthusiastically given or when non-compliant the time out procedure was used appropriately until Jackson was compliant.
Results
The family completed four CDI sessions and five PDI sessions (including the two teach sessions) for a total of nine PCIT sessions. PCIT usually varies between 12 and 14 sessions but length can be variable and is dependent on parent skill acquisition [6]. Jackson’s parents were highly motivated and were both consistent in their daily practice of the skills at home, which is the most likely explanation for their shorter than average length of therapy.
ECBI scores
Initial ECBI Scores were clinically elevated (T greater than or equal to 60) for both his father and step mother in both intensity and problem, but more elevated for his step mother. As therapy progressed, ECBI scores consistently declined (Figure 1). At the end of treatment both ECBI problem and intensity scores were below clinically significant level for Jackson’s father and step mother.
Figure 1: The Eyeberg Childhood Behavior Inventory T-Scores were charted at each treatment visit for both father and step mother. Intensity score measure refers to the frequency of a behavior. The problem score measure refers to whether or not the parent considers the behavior a problem. T scores greater than or equal to 60 were considered to be clinically significant for conduct disordered behavior. C: CDI Session and P: PDI Session. S. Eyeberg and D. Pincus, 1999, The Eyeberg Child Behavior Inventory.
CDI skills
Both parents improved their PRIDE skills during the CDI phase. Jackson’s father met mastery criteria for PRIDE skills (do skills) during his first CDI session, but had more than three questions (don’t skill) which prevented him from achieving mastery in the first session. He met full mastery criteria for CDI during his third CDI Session. Jackson’s step mother met mastery criteria for reflections during the first CDI session and achieved mastery of all CDI skills during the third CDI session.
Behavioral Observations
Behavioral Observations during the initial CDI sessions with Jackson’s father showed Jackson smiling, laughing, hugging and sitting close to his father. Jackson showed enthusiasm by talking and providing detailed descriptions of his play and imagination to his father. During transitions between play with his father and stepmother Jackson exhibited clinging and crying during separation from his father, suggesting an insecure and anxious attachment. During initial CDI sessions with his stepmother, Jackson exhibited a flat and emotionless affect, demonstrated much less talking and enthusiasm during play, and did not show affection or warmth towards his step mother; suggesting an avoidant attachment. During play with his stepmother, there were frequent requests for his father to return and on some occasion’s attempts to escape from the room when these requests were not responded to. From the beginning, both of Jackson’s parents demonstrated enthusiasm in their play with Jackson by providing frequent descriptions of his play and praising him for desired behaviors. As CDI sessions continued Jackson began demonstrating increased verbalizations, eye contact, and interest during his play with his stepmother. By the end of treatment Jackson was enthusiastic and excited to play with his step mother and no longer whined or requested his father to return after transition to play with his to be step-mother. Towards the end of treatment he demonstrated more affection by sitting close to her and smiling and laughing with her, suggesting he had developed a more secure attachment with her.
Discussion
This case study describes the successful use of PCIT with a five year old parentally bereaved child experiencing symptoms of insecure attachment, anxiety and depression and exhibiting aggressive and disruptive behaviors, a presentation more commonly seen in younger boys [23]. Treatment was associated with clinically significant reductions in Jackson’s disruptive, aggressive, and non-compliant behaviors and difficulties with separating from his father. Parents and teachers also informally reported observations of decreased disruptive behaviors, attention problems, and separation difficulties both at home and school. Behavioral observations during PCIT sessions showed Jackson exhibited less distress during transitions out of activities that involved his father and separation from his father. During interaction with his step-mother Jackson showed increased verbalizations during play, increased enthusiasm and affection, and extinguishment of whining for his father and elopement during play sessions with his step-mother.
During the CDI phase of treatment Jackson’s father and step mother used the PRIDE skills to increase the protective factor of positive parenting by demonstrating increased parental warmth and sensitivity to Jackson’s needs and providing attention for positive behaviors. During PDI they maintained the positive parenting skills learned in CDI, while providing effective discipline. According to the transitional events model, positive attention, parental warmth, increased selfesteem and effective discipline are all protective factors against maladjustment and psychopathology in parentally bereaved children [24,34,45].
Introduction of a step-parent is an event that is experienced by both children of divorced parents and parentally bereaved children if a surviving parent decides to re-marry. The literature has identified this as a stressful and often negative event that is usually resisted by the child [46,47]. When Jackson began treatment his step-mother was experiencing more behavioral problems with him and her ECBI scores were more elevated. This suggests that Jackson was resistant to forming a relationship with her and felt insecure in his attachment with her. Bowlby assumed that role of a surrogate attachment figure (i.e. step parent) can provide a secure attachment for a child if they demonstrate a high degree of warmth, responsiveness to the child’s needs and sensitivity to their signals [16,17]. During CDI Jackson’s stepmother learned and increased her use of the PRIDE skills. These skills allowed
her to demonstrate a high degree of warmth and responsiveness to Jackson, which is associated with forming a more secure attachment and increased self-esteem. As treatment progressed Jackson began sitting closer to his step-mother, increasing his verbalizations and eye contact with her, and demonstrated less clinging, whining and attempts to escape while playing with her [17].
Previous research has identified that parentally bereaved children are not easily identifiable or accessible [23]. This case study provides an opportunity observe and describe the behavioral difficulties of a parentally bereaved preschooler and his interactions with his father and step mother. This study describes the potential theoretical links between the parental bereavement literature and the PCIT literature. It discusses how PCIT operationalizes the theoretical protective factors identified in the literature into measurable treatment outcomes. This case study also describes how PCIT was used specifically in a situation where a step parent was being introduced, which provides evidence for future research into this separate population. These preliminary findings suggest that PCIT may be an effective intervention for young parentally bereaved children [48-52].
Although findings of this case study serve as preliminary evidence supporting the use of PCIT with parentally bereaved children it has significant limitations. The first and foremost limitation of this study is the case study design which lacks multiple subjects, randomization and control group comparison. For this reason I cannot determine whether the findings were actually due to PCIT treatment, or were a result of the passage of time or some other unidentified variable. Another identified limitation was the use of informal behavioral reports from teachers during treatment instead of collecting more objective data from the teachers during treatment; as was done with the parents using the ECBI. A final limitation was the lack of formal re-evaluation and the end of treatment, by both the parents and teachers, to provide objective data to evaluate the perceived reduction in anxious/ depressive, attention, withdrawn and aggression symptoms.
Future research should focus on implementing studies with larger samples, randomization, and experimental design to help establish PCIT as an effective intervention for parentally bereaved children and those adjusting to the introduction of a step-parent. These preliminary findings suggest that PCIT offers potential to provide a much needed bridge in the current practice gap for young parentally bereaved children, but additional research is needed to support these promising preliminary findings.
References
- Eyeberg S, Robinson EA (1982) Parent-child interaction training: Effects on family functioning. Journal of Clinical Child Psychology pp: 130-137.
- Einstadt TH, Eyeberg S, McNeil CB, Newcomb K, Funderburk B (1992) Parent-child interaction therapy with behavior problem children: Relative effeciveness of two stages and overall treatment outcomes. Journal of Clinical Child Psychology pp: 42-51.
- Foote R, Schuhmann E (1998) Parent-child interaction approaches to treatment of child behavior problems. Advances in Clinical Child Psychology pp: 125-151.
- Neary EN, Eyeberg S (2002) Mangement of disruptive behavior in young children. Infants and Young Children pp:53-67.
- Brestan EV, Eyberg SM (1998) Effective psychosocial treatments of conduct-disordered children and adolescents: 29 years, 82 studies, and 5,272 kids. J Clin Child Psychol 27: 180-189.
- Gallagher N (2003) Effects of parent child interaction therapy on young children with disruptive behavior disorders. Bridges: Practice Based Research Syntheses 1:4.
- Choate ML, Pincus DB, Eyeberg S, Barlow DH (2005) Parent-child interaction therapy for treatment of separation anxiety disorder in young children: A pilot study. Cognitive and Behavioral Practice 12: 126-135.
- Pincus DB, Santucci LC, Ehenreich JT, Eyeberg SM (2008) The implementation of parent-child interactional therapy for youth with separation anxiety disorder. Cognitive Behavioral Practice 15: 118-125.
- Eyberg SM, Nelson MM, Boggs SR (2008) Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. J Clin Child AdolescPsychol 37: 215-237.
- Ware LM, Forston BL, McNeil CB (2003) Parent-child interaction therapy: a promising intervention for abusive families. The Behavior Analyst Today 3: 375-382.
- Solomon M, Ono M, Timmer S, Goodlin-Jones B (2008) The effectiveness of parent-child interaction therapy for families of children on the autism spectrum. J Autism DevDisord 38: 1767-1776.
- Wagner SM, McNeil CB (2008) Parent-child interaction therapy for ADHD: A critical overview and critical literature review. Child & Family Behavior Therapy pp: 231-256.
- Archer J (1999) The nature of grief: The evolution of psychology and reactions to loss. Routlege 2: 119-121.
- Institute of Medicine Committee for the Study of Health Consequences of the Stress of Bereavement (1984) Bereavement, reactions, consequences and care. Washington DC: National Academic Press.
- Horn PV, Liberman AF (2009) Using dydadic therapies to treat traumatized young children. In D Brom, P Pat-Horenczyk, Ford J, Treating traumatized children: Risk, reslilence and recovery pp: 210-24.
- Bowlby J (1988) A secure base: Clinical applications for attachment theory. New York: Routledge.
- Ainsworth MD (1989) Attachments beyond infancy. Am Psychol 44: 709-716.
- Siegel DJ (1999) The developing mind: How relationships and the brain interact and shape who we are. New York: Guilford Press pp: 66-120.
- Lehman DR, Lang EL, Wortman C, Sorenson SB (1989) Long-term effects of sudden bereavement: Marital and parent-child relationships. Journal of Family Psychology pp: 344-367.
- Thompson MP, Kaslow NJ, Price AW, Williams K, Kingree JB (1988) Role of secondary stresses in parental death-child distress relations. Journal of Abnormal Psychology 26: 357-366.
- Ellis J, Dowrick C, Lloyd-Williams M (2013) The long-term impact of early parental death: lessons from a narrative study. J R Soc Med 106: 57-67.
- Worden JW, Silverman PR (1996) Parental death and the adjustment of school-age children. Omega: Journal of Death and Dying pp: 219-230.
- Dowdney L, Wilson R, Maughan B, Allerton M, Schoenfield P, et al. (1999) Psychological disturbance and service provision in parentally bereaved children: Prospective case control study. British Medical Journal 319: 354-357.
- Haines RA, Ayers TS, Sandler IN, Wolchik SA (2008) Evidence-based practices for parentally bereaved children and their families. Prof Psychol Res Pr 39: 113-121.
- Sandler IN, Ayers TS, Wolchik SA, Tein JY, Kwok OM, et al. (2003) The family bereavement program: efficacy evaluation of a theory based prevention program for parentally bereaved children and adolescents. J Consult Clin Psychol 71: 587-600.
- Kranzler EM, Shaffer D, Wasserman G, Davies M (1990) Early childhood bereavement. J Am Acad Child Adolesc Psychiatry 29: 513-520.
- Willis CA (2002) The grieveing process in children: Strategies for understanding, educating and reconciling children's perceptions of death. Early Childhood Education Journal pp: 221-227.
- Nickerson A, Bryant RA, Aderka IM, Hinton DE, Hoffman SG (2013) The impacts of parental loss and adverse parenting on mental health: Findings from the national comorbidity replication survey. Psychological Trauma Theory, Research and Practice and Policy 5: 119-127.
- Felner RD, Terre L, Rowlinson RT (1988) A life transistion framework for understanding marital dissolution and family reorganization. In S. Wolchik, & P. Karoly, Children of divorce: Empirical perspectives on adjustment. New York: Gardner pp: 35-65.
- Sandler IN, Gersten J, Reynolds K, Kalgren C, Ramirez R (1988) Using theory and data to plan interventions: Designing a program for bereaved children. In B. Gottleib, Marshalling Social Support: Formats, processes, and effects. Thousand Oaks: Sage Publications pp: 53-83.
- Wolchik SA, Tein JY, Sandler IN, Ayers TS (2005) Stressors, quality of the child caregiver relationship and children's mental health problems after parental death: The mediating role of self-esteem Beliefs. J Abnorm Child Psychol 34: 221-238.
- Haine RA, Ayers TS, Sandler IN, wolchik SA, Weyer JL (2003) Locus of control and self esteem as stresss moderators of stress mediatros in parentally bereaved children. Death Studies pp: 619-640.
- Sanders MR, Cann W, Markie-Dadds C (2003) Triple P positive parenting program: A universal population-level approach to the prevention of child abuse. Child Abuse Review 12:151-171.
- Haine RA, Wolchik SA, Sandler IN, Millsap RE, Ayers TS (2006) Positive parenting as a protective resource for parentally bereaved children. Death Stud 30: 1-28.
- Tein JY, Sandler IN, Ayers TS, Wolchik SA (2006) Mediation of the effects of the family bereavement program on mental health problems of bereaved children and adolescents. PrevSci 7: 179-195.
- Kwok OM, Haine RA, Sandler IN, Ayers TS, Wolchik SA, et al. (2005) Positive parenting as a mediatior of the relations between parent psychological distress and mental health problems of parentally bereaved children. J Clin Child AdolescPsychol 34: 260-271.
- Sandler I, Balk D, Jordan J, Kennedy C, Nadeau J, et al. (2005) Bridging the gap between research and practice in bereavement: report from the Center for the Advancement of Health. Death Stud 29: 93-122.
- Cohen JA, Mannarino AP, Knudsen K (2004) Treating childhood traumatic grief: a pilot study. J Am Acad Child Adolesc Psychiatry 43: 1225-1233.
- Tonkins SA, Lambert MJ (1996) A treatment outcome study of bereavement groups for parentally bereaved children. Child and Adolescent Social Work Journal pp: 3-21.
- Eyeberg SM, Boggs SR, Algina J (1995) Parent-child interaction therapy: A psychosocial model for the treatment of young children with conduct disorders. Psychopharmacol Bull 31: 83-91.
- Achenbach TM, Rescorta LA (2000) Manual for the ASEBA Preschool Forms & Profiles. Burlington: Achenbach System of Empirically Based Assessment.
- Eyeberg SM, Pincus DM (1999) Eyeberg Child Behavior Inventory. Lutz: PAR, INC.
- Eyeberg SM, Nelson MM, Duke M, Boggs SR (2004) Manual for the dydadic parent-child interaction coding system (3rd eds). Thousand Oaks: Sage Publications.
- Eyeberg SM, Funderburk BW (2011) Parent-child interaction therapy protocol. Gainesville: PCIT International.
- Sandler IN, Wolchik SA, Mckinnon D, Ayers TS, Roosa MW (1997) Developing linkages between theory and intervention in stress and coping processes. In SA Wolchik SA. Sandler, Handbook of children's coping. New York: Plenum Press pp: 3-40.
- Doyle KW, Wolchik SA, Dawson-McClure S (2002) Development of the stepfamily events profile. J FamPsychol 16: 128-143.
- Fast I, Cain AC (1966) The stepparent role: potential for disturbances in family functioning. Am J Orthopsychiatry 36: 485-491.
- Campbell SB (1997) Behavior problems in preschool children: Developmental and family issues. Advances in Clinical Child Psychology pp: 1-26.
- Herschell AD, Calzada EJ, Eyeberg SM, McNeil CB (2002) Parent-child interaction therapy: New directions for research. Cognitive and Behavioral Practice 9: 9-16.
- Sandler IN, West SG, Baca I, Pillow DR, Gersten JC, et al. (1992) Linking empirically based theory and evaluation: The family bereavement program. American Am J Community Psychol 4: 491-521.
- Timmer SG, Urquiza AJ, Zebell N (2006) Challenging foster caregiver-maltreated child relationships: The effectiveness of parent-child interaction therapy. Children and Youth Services Review 28: 1-19.
- Doyle KW, Wolchik SA, Dawson-McClure S (2002) Development of the stepfamily events profile. J FamPsychol 16: 128-143.
Citation: Franke RK (2016) Parent-Child Interaction Therapy: Case Study of Application to a Parentally Bereaved Child. J Child Adolesc Behav 4: 293. Doi: 10.4172/2375-4494.1000293
Copyright: © 2016 Franke RK. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 14820
- [From(publication date): 6-2016 - Apr 25, 2024]
- Breakdown by view type
- HTML page views: 13941
- PDF downloads: 879