Comparison of Child and Parent Cognitive Behaviour Therapy on Reduction of Attention Deficit Hyperactivity Disorder Symptoms in Children
Received: 20-Oct-2015 / Accepted Date: 07-Mar-2016 / Published Date: 14-Mar-2016 DOI: 10.4172/2375-4494.1000285
Abstract
Objective: Attention deficit hyperactivity disorder (ADHD) is a common early-onset childhood disorder that is introduced by attention deficiency, hyperactivity and impulsivity. The aim of this study was to compare the effect of parent and child Cognitive Behaviour therapy in reduction of symptoms of ADHD in 7 to 12 aged children. Method: This research is performed in the scope of semi-experimental research. For testing the above phenomenon a sample were selected including 50 children, referred to child and adolescent psychiatry clinic who were suffering from ADHD on the basis of the recognition of the psychiatrist and according to the questionnaire prepared specially to diagnose this type of interference DSM-IV-TR. Then the sample randomly assigned in to three groups, 17 parent CBT group, 18 child CBT group and 15 control group. The parents and children in the experimental groups were subjected to cognitive and behavioural therapy for 8 sessions each for 1.5 hour. Treatment outcomes were assessed using the DSM-IV-TR questionnaires which were filled by teacher and parents of the children suffering from ADHD at baseline week 1, 4 and 8. For the purpose of data analysis I have used the one- way analysis variance (ANOVA). Results: The results from analyzing the data obtained from the research showed that at the end of the therapy, in cognitive and behavioural groups reduction of attention-deficiency and hyperactivity was significant p ≤ 0.02 in children suffering from ADHD in comparison with the control group. Conclusions: we can conclude that parent and child based cognitive behaviour therapy will affect the decrease of attention-deficiency and hyperactivity in these children and it is suggested that the specialists and psychologists can also use drug therapy along with the other common treatments as a complementary therapy for decreasing the mentioned symptoms in children suffering ADHD.
Keywords: Attention deficit hyperactivity disorder; Child cognitive behaviour therapy; Drug therapy; Parent cognitive behaviour therapy
Introduction
Attention-Deficit Hyperactivity Disorder (ADHD) is an etiologically complex, highly heritable, common childhood psychiatric disorder [1] in children and adolescents [2-5], also ADHD is a neurodevelopmental disorder [6] that the core features according to the Diagnostic and Statistical Manual of Mental Disorder–Fourth Edition (DSM-IV-TR) are characterized by symptoms of inattention, hyperactivity and impulsivity [2,4,7-13]. In DSM-IV, the diagnostic criteria required impairment in social, academic, or occupational functioning. With DSM-5 publication imminent in 2013, further evaluation of impairment in ADHD is timely [14,15].
ADHD has traditionally been considered a childhood disorder, but there is accumulating evidence for the validity of the diagnosis in adulthood [16] Over the past ten years, an increasing number of children have been diagnosed with attention deficit hyperactivity disorder and some reports suggest that the prevalence rate of the disorder is as high as 11% [17] it is estimated to affect 3% to 7% of school-aged children in the United States [6]. ADHD has three subtypes: predominantly inattentive type (ADHD-I), which accounts for 45% of all ADHD patients; predominantly hyperactive-impulsive (ADHD-H), which affects 21% of all patients; and combined-type (ADHD-C), which occurs in 34% of all patients [18,19].
Inattention, hyperactivity and impulsivity are the most important difficulties that can destroy the relationship between child and parents, teachers and classmates [8,10,17]. This will make parents hopeless because they do not know how to do after their child behaviour [8].
Along with these general come several specific deficits that can severely impact a child’ ability to function successfully in several domains of daily life. This leads mental health professionals and researchers to explore the best practices for helping children with ADHD become successful in their home, school and social environments [12].
Some therapies in this disorder are more important and beneficial like a) medical therapy, b) behaviour therapy, c) cognitive-behaviour therapy [2,20].
Without early intervention, children with ADHD can experience negative long-term effects as adults, such as lower levels of education and more arrests [17].
Medications are the most effective single treatment for individuals with ADHD of all ages. However, medications alone may represent insufficient treatment for many adults with ADHD. Consequently, various adjunctive treatments for ADHD have been developed, with cognitive behavioural therapy (CBT) emerging as a particularly promising one [6]. It is imperative that elementary school counsellors be aware of specific interventions that may use to help decrease the ADHD symptoms that negatively impact student learning [17]. Views about the appropriateness and anticipated effects are strong predicators of willingness to use psychiatric medications for children [20].
Recent decade of 1950, cognitive behaviour therapy (CBT) was introduced for many difficulties like aggressive controlling, ADHD, eating disorders, marital difficulties up to schizophrenic disorders. Researches indicate that CBT can be beneficial therapy for many psychological problems and psychiatry disorders [21]. In recent years, cognitive training has been investigated as a potential ADHD treatment [22]. About 10% to 20% of children in school age suffer from attention deficit hyperactivity disorder that 1 or 2 million of 20 million students in Iran have this problem [23].
The main goal of CBT in ADHD children is to learn them that they can answer their problems themselves. This aim will not obtain by drug therapy but by educating children to use rules in daily life and relationship with others, we can make them more able.
This is the first randomized controlled trial to compare the efficacy of child and parent CBT protocol for children with a diagnosis of ADHD.
Method
Trial organization
This was an 8-week, parallel group, randomized trial undertaken in out-patient child and adolescent clinic, between October 2013 and April 2014.
Participants
Inclusion criteria
Participants are (self) referrals seeking treatment for their children ´s ADHD at the child and adolescent psychiatry clinic. To be eligible for the study, patients have to meet the following inclusion criteria: after intake allocated to outpatient treatment unit, aged 7-12 years, DSM-IV-TR diagnosis of ADHD .Patients with other behavioral disorders are not included.
Exclusion criteria
Patients with severe neurological or psychiatric disorders (e.g. psychosis, bipolar disorder) requiring medication, are excluded from the study. If children had been previously diagnosed with mental retardation (IQ < 70) also excluded. In addition, patients were excluded if they had a clinically significant chronic medical condition, including organic brain disorder, seizures, current abuse or dependence on drugs within the last six months. Patients currently using ADHD medication (e.g. methylphenidate) are allowed to participate provided that they are on a stable dose and no medication changes are planned for the duration of the trial .To participate, parents and children had to be willing to comply with all requirements of the study.
Study design
Patients underwent a standard clinical assessment comprising a psychiatric evaluation and a structured diagnostic interview. Then 50 family availably with children by ADHD randomized to receive therapy. All study subjects were randomly assigned to one of three groups: group 1, 17 parents received CBT, group 2, 18 children receive CBT, group 3, 15 control group (only drug therapy). Every group´s children receive drug. After a description of the procedures and purpose of the study we test groups by DSM-IV-TR checklist primarily. Experimental groups trained 8 sessions 1.5 hour weekly cognitive behaviour therapy. At last training groups re-examined by pre-test.
Treatment protocols
Parent CBT group
The treatment program focuses on the training of coping skills and on symptom management strategies. It consists of 8 sessions, the first session parents report anxious about their child. In second and third sessions we investigate the thought and behavior then we challenge improperly thought and behavior. Other two sessions focus on problem solving and using this skill with children in different situations. After every session we gave working at home. Next two sessions focus on behavior controlling and child depriving to promote parents skills. At the last session we solve parent problems about training skills.
Children CBT group
Participants in children group receive an integrated treatment for ADHD, combining the main elements of the CBT program for ADHD .The treatment program focuses on the training of coping skills and on symptom management strategies. It consists of 8 sessions that focuses on psycho-education about ADHD and several organization and planning skills, such as using a plan, problem solving by generating alternatives and picking the best solution, and breaking down complex or overwhelming tasks into smaller steps, recognition of external and internal signs in problems, reducing distractibility by removing sources of distraction during a task, using cognitive restructuring, adaptive thinking and internal speech, notice physical symptoms of nervousness. We had optional modules involve to tackle procrastination and cooperate with others.
Assessment
The ADHD rating scale is used as the measure for severity of ADHD symptoms, DSM-IV-TR Persian version [10]. In the Persian version, the ADHD rating scale is 18 item self-report questionnaires in which each item is scored on a 4-point scale ranging from 0 to 3. The children were diagnosed as ADHD according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders, fourth edition revised (DSM-IV-TR) [7] by experienced child psychiatrists. The diagnosis was based on clinical interviews with a psychiatrist, school reports, the Conners Global Index Teacher version (CGI-T) [24] and the Conners Global Index Parent version (CGIP) [25].
Statistical analysis
A one-way analysis of variance with a two-tailed post-hoc Tukey mean comparison test were performed on the change in DSM-IV-TR ADHD Rating scale scores from baseline. Results are presented as mean ± standard error of the mean (SEM) differences and were considered significant with p ≤ 0.02.
Results
No significant differences were identified between clients randomly assigned to group 1, 2 and 3 with regard to basic demographic data including age, gender and ethnicity (Table 1).
| Parent CBT Group | Children CBT Group | Control Group | |
|---|---|---|---|
| Girl | 2 | 6 | 6 |
| Boy | 14 | 11 | 9 |
| Age (mean ± SD ) | 9. 37 | 9.70 | 9 .33 |
| Ethnicity | All Persian | All Persian | All Persian |
Table 1: Baseline data; demographic characteristics.
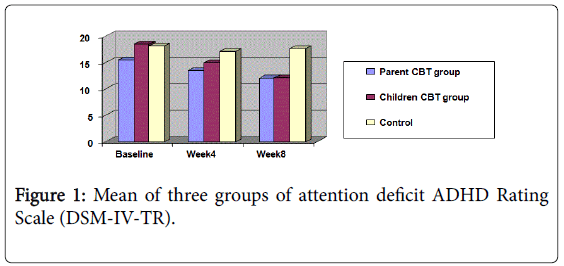
ADHD Rating Scale (DSM-IV-TR): The mean of three groups of patients in attention deficit are shown in Figure 1. There were no significant differences between three groups at baseline on the ADHD Rating Scale (DSM-IV-TR). Both parent CBT group and children CBT group showed a significant improvement over the 8 weeks of treatment.
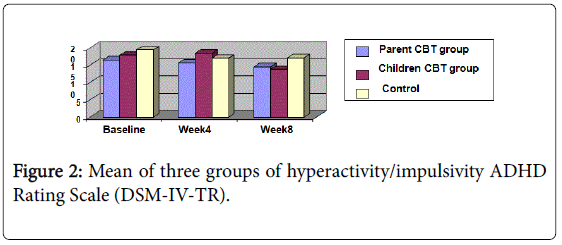
The mean of three groups of patients in hyperactivity and impulsivity are shown in Figure 2. There were no significant differences between three groups at baseline on the ADHD Rating Scale (DSMIV- TR). Both parent CBT group and children CBT group showed a significant improvement over the 8 weeks of treatment.
A one-way analysis of variance and a two-tailed post-hoc Tukey mean comparison test are shown in Tables 2 and 3. There were no significant differences between three groups in first and fourth week but in 8 week there were significant differences (p ≤ 0.02) between groups. So post-hoc Tukey mean comparison performed that showed there were significant differences between parent CBT group and control group (Drug therapy). There were significant differences between children CBT group and control group (Drug therapy). But didn´t show significant differences between two experimental groups. It means the differences between parent CBT group and children CBT group were not significant.
| Scale: DSM IV TR | Variance source | CS | df | MS | F | P |
|---|---|---|---|---|---|---|
| baseline | Between groups | 190.969 | 2 | 95.484 | 1.008 | 0.373 |
| In groups | 4264.010 | 45 | 94.756 | |||
| All | 4454.978 | 47 | ||||
| Week4 | Between groups | 216.436 | 2 | 108.218 | 0 841. | 0 438. |
| In groups | 5792.608 | 45 | 128.725 | |||
| All | 6009.045 | 47 | ||||
| Week 8 | Between groups | 799.414 | 2 | 399.707 | 3.985 | 0 026. |
| In groups | 4513.751 | 45 | 100.306 | |||
| All | 5313 . 165 | 47 |
Table 2: ANOVA scores of three groups in ADHD Rating Scale (DSMIV- TR).
| Group | Group | Mean differences | Error | P | |
|---|---|---|---|---|---|
| Week 8 | parent CBT group | children CBT group | 7826. | 3.48847 | 0.973 |
| parent CBT group | Drug Therapy | 8-.3735(*) | 3.59946 | 0.052 | |
| children CBT group | Drug Therapy | 9-.1561(*) | 3.54787 | 0.035 |
Table 3: A two-tailed post-hoc Tukey mean comparison test between groups in week 8.
Discussions
The aim of this research was comparing the effectiveness of parent and child CBT therapy in reduction of Attention deficit hyperactivity disorder symptoms. We said that ADHD affects 3% to 5% of schoolage children [26]. ADHD is commonly considered a disorder that affects children and adolescents; however follow-up studies indicate significant continuation and impairment into adulthood [27]. Researches show if ADHD didn´t diagnose and therapy would have difficulties for family, teachers and society. Just using drugs can solve one aspect not all problems of ADHD children [28]. Attitudes toward pharmacological treatment may be a major factor contributing to adherence to such treatment [29]. In response to these concerns, it is critical that further development of psychosocial interventions for young children with ADHD be pursued. In part, this suggestion follows from the conjecture that interventions may be the most effective with young children, who have not yet experienced school failure, social rejection, and a long history of negative parenting responses to their disruptive behaviours [30].
Many studies have reported impaired family functioning related to ADHD [31]. Thus, parent practices and family relationships are important for the developmental course and treatment outcomes of ADHD [32,33]. Among psychosocial interventions, parent training to help parents learn and implement behavioural treatment has the strongest evidence base showing positive effects for school age children with ADHD [34]. For preschool children with ADHD, parent training in behaviour management is an especially helpful and the most appropriate psychosocial intervention [35,36]. When children are young, parents have an enormous impact on their child's behaviour creating a window of opportunity to teach parents how to be positive and consistent in their parenting responses, help reduce noncompliant and aggressive behaviours, and help their child persist at a difficult task and provide successful experiences for their child, thus reducing risk for continued problems in later years [37]. There have been a few studies in which behavioural management techniques have been applied within the preschool setting to treat individual preschool children presenting with hyperactive, inattentive and disruptive behaviours. We identified four published case series [37,38] and two single-case reports [38] All studies reported improved task-related attention and ability to delay activities and decreased disruptive behaviours.
Results of present research show that parent CBT group and children CBT group in reduction of attention deficit/hyperactivity disorder. It’s mean the therapy protocols performed as effective variables reduce ADHD´s signs as dependent variables, but results didn´t show significant differences between two management group and children cognitive therapy group. There is considerable evidence that parent, child, and parent-child interventions can reduce problem behaviours in young children displaying a range of disruptive behaviours, including excessive hyperactivity and inattention [37]. Whereas Pelham said by Alizadeh [23] performing psychosocial therapy like parent therapy for children by ADHD is more helpful. Corrin [39] observed the efficacy of parent and children’s therapy together is more than lonely. Generally some researches that trained children and parent together receive more positive results [21]. Recent studies show positive effects of cognitive behavioural therapy (CBT) in ADHD patients three recent randomized controlled trials reported a positive effect of CBT in adult ADHD patients without substance abuse [40-42]. In the study by Safren et al. [41], 86 adult ADHD patients with residual ADHD symptoms during medication treatment were randomized to individual CBT or to relaxation as a control condition. Assessments of ADHD symptoms by blinded investigators took place at baseline, post-treatment, and at 6 months and 12 months follow up. CBT resulted in a significant greater reduction of ADHD symptoms than relaxation therapy, both post-treatment and at 1 year follow up. In another study, Solanto et al. [43] investigated a meta-cognitive group therapy designed to improve time management, organization and planning in adults with ADHD.
Interventions for high-risk children in this age range are crucial because they can set either a firm or fragile foundation for later development, learning, and attitudes about school. Intervening early to remediate these difficulties may have lifelong benefits for enhancing children's later success. Research such as this, which provides empirical information about ways to change key risk variables, can provide the basis for early intervention plans for schools, which will benefit children at high risk for later school difficulties and conduct problems [30].
Limitations
The study suggest that parent cognitive behavior therapy and child cognitive behavior therapy may be useful for ADHD, however our study is small we didn´t control co-morbid disorders that may effect on therapy. One patient in parent CBT group because of some difficulties(mother´s divorcement) didn´t complete training sessions and one in children CBT group because distance of child´s residence was far from clinic didn´t continue therapy. Our results would need to be confirmed in a large randomized controlled study. Lastly, we did not look separately at ADHD subtypes and it is possible that the scores of child therapy and parent therapy measures differ in patients with various ADHD subtypes. Future studies should more carefully consider differences across ADHD subtypes. Most families ascertained in this sample were not complete trios as there were many single parent families (mostly mothers). This limits power to examine whether parent training in ADHD has more or less influence on child clinical presentation compared to only mother training.
Conclusion
In summary, the combined parent therapy and child therapy interventions showed that psycho-social interventions can help to reduce hyperactive, inattentive, and oppositional behaviors among young children with a primary diagnosis of ADHD [30]. Overall, we can conclude that parent and child based cognitive behaviour therapy will affect the decrease of attention-deficiency and hyperactivity in these children and it is suggested that the specialists and psychologists can also use methylphenidate (MPH) as drug therapy along with the other common complementary treatment for decreasing the mentioned symptoms in children suffering ADHD. However, Pharmacotherapy is considered the first-line treatment for ADHD in children and adolescents [44] and methylphenidate is the most common treatment of attention deficit hyperactivity disorder in children [45], literature shows, families who received combined parent and child training exhibited both cross setting changes and greater maintenance of treatment effects at one-year follow-up [30].
Acknowledgement
First of all, the authors wish to thanks all of the children and the parents who participated into the study and also Dr. Mohammadi’s psychiatry clinic staffs for invaluable helps.
References
- Choudhry Z, Sengupta SM, Grizenko N, Harvey WJ, Fortier MÈ, et al. (2013) Body weight and ADHD: examining the role of self-regulation. PLoS One 8: e55351.
- Akhondzadeh S, Mohammadi MR, Momeni F (2005) PassifloraIncarnata in the Treatment of Attention/Deficit Hyperactivity Disorder in Children and Adolescent. pp: 609-614.
- Mohammad Esmail E (2006) Handbook of Cognitive-Behavioral Therapy for Children with Attention Deficit Hyperactivity Disorder.
- Amiri S, Mohammadi MR, Mohammadi M, Nouroozinejad GH, Kahbazi M, et al. (2008) Modafinil as a treatment for Attention-Deficit/Hyperactivity Disorder in children and adolescents: a double blind, randomized clinical trial. ProgNeuropsychopharmacolBiol Psychiatry 32: 145-149.
- Mohammadi MR, Kashani L, Akhondzadeh S, Izadian ES, Ohadiani S (2004) Efficacy of Theophylline Compared to Methylphenidate for the Treatment of Attention/Deficit Hyperactivity Disorder in Children and Adolescent: a Pilot Double –Blind Randomized Trial. J Clin Pharm Ther29: 139-144.
- Ramsay j, Russell (2010) CBT far Adult ADHD. University of Pennsylvania School of Medicine. Journal of Cognitive Psychotherapy 24: 37-45.
- American Psychiatric Association Diagnostic and statistical manual of mental disorders (2000) Text orevision (DSM-IV-TR) Author; Washington DC.
- Barton J (2006) Attention/Deficit Hyperactivity Disorder in Children:Practical Help for Parents.
- Mohammadi MR, Ghanizadeh A, Alagheband-Rad J, Tehranidust M, Mesgarpur B, et al. (2004) Selegiline in Comparison with Methylphenidate in Attention/Deficit Hyperactivity Disorder Children and Adolescent in a Double –Blind Randomized Clinical Trial. J Child AdolescPsychopharmacol14: 418-425.
- Delavar A, Mohammadi MR, Hooshyar Z (2008) The Constructional Norm – Finding of a Rating Scale for Diagnosing Attention/Deficit Hyperactivity Disorder in Children. Iranian J Pcychiatry 3:9-15.
- Mahone EM, Hoffman J (2007) Behavior ratings of executive function among preschoolers with ADHD. Clin Neuropsychol 21: 569-586.
- Lerew CD (2003) The Use of a Cognitive Strategy as an Academic and Behavioral Intervention for Children with Attention Deficit Hyperactivity Disorder.
- Akhondzadeh S, Mohammadi MR, Khademi M (2004) Zinc sulfate as an adjunct to methylphenidate for the treatment of attention deficit hyperactivity disorder in children: a double blind and randomized trial ISRCTN64132371. BMC Psychiatry 4: 9.
- Nigg JT (2013) Attention-deficit/hyperactivity disorder and adverse health outcomes. Clin Psychol Rev 33: 215-228.
- Zelazny K, Simms LJ (2015) Confirmatory factor analyses of DSM-5 posttraumatic stress disorder symptoms in psychiatric samples differing in Criterion A status. J Anxiety Disord 34: 15-23.
- ArntsbergGrane V, Endestad T, Pinto AF, Solbakk AK (2014) Attentional Control and Subjective Executive Function in Treatment-Naive Adults with Attention Deficit Hyperactivity. Disorder PLoS One 9: e115227.
- Mark R, Crundwell A (2007) An Initial Investigation of the Impact of Self –Regulation and Emotionality on Behavior Problems in Children with ADHD. Canadian Journal of School Psychology 20: 62-74.
- Gong J, Yuan J, Wang S, Shi L, Cui X, et al. (2014) Feedback-related negativity in children with two subtypes of attention deficit hyperactivity disorder. PLoS One 9: e99570.
- Schottelcorb A, Ray DC (2009) ADHD Symptom Reduction in Elementary students: a Single Case Effectiveness Design. American School Counselor Association 13: 11-22.
- Dos Ries S, MychailszynMP, Evans Lacho, Beltran A, RileyAW,et al. (2009) The Meaning of Attention/Deficit Hyperactivity Disorder Medication and Parent´s Initiation and Continuity of Treatment for Their Child. J Child AdolescPsychopharmacol 19:377-383.
- Paul S (2005) A Clinical Guide to Think Good-Feel Good: Using CBT with Children and Young People.
- Cortese S, Ferrin M, Brandeis D, Buitelaar J, Daley D, et al. (2015) Cognitive Training for Attention-Deficit/Hyperactivity Disorder: Meta-Analysis of Clinical and Neuropsychological Outcomes from Randomized Controlled Trials J Am Acad Child Adolesc Psychiatry 54: 164-174.
- Alizadeh H, Andries C (2002) Interaction of Parenting styles and Attention Deficit Hyperactivity Disorder in Iranian Parents .Child and Family Behavior Therapy 24: 37-52.
- Conners CK, Sitarenios G, Parker JD, Epstein JN (1998b) Revision and restandardization of the Conners Teacher Rating Scale (CTRS-R): Factor structure, reliability, and criterion validity. J Abnorm Child Psychol26: 279-291.
- Conners CK, Sitarenios G, Parker JD, Epstein JN (1998a) The revised Conners’ Parent Rating Scale (CPRS-R): factor structure, reliability, and criterion validity. J Abnorm Child Psychol26: 257-268.
- Seyed EA,Hussein SA (2010) Increase in Teacher´s Knowledge about ADHD after a Week Long Training Program. J AttenDisord13: 420-423.
- Mitchell JT, Nelson–Gray RG, Anastopoulos A (2008) Adapting an Emerging Empirically Supported Cognitive Behavioral Therapy for Adult with ADHD and Co morbid Complications. Clinical Case Studies 11: 423-448.
- Sadock BJ, Sadock VA, Kaplan, Sadock’s (2005) Comprehensive Textbook of Psychiatry. (8th edn.) Lippincott William& Wilkins.
- Berger I, Nevo Y, dor T, GoldsweigG (2008) Attitude Toward Attention/Deficit Hyperactivity Disorder ( ADHD ) Treatment: Parent and Children´s Perspectives. J Child Neurol23: 1036 -1042.
- Webster-Stratton CH, Reid MJ, Beauchaine T (2011) Combining parent and child training for young children with ADHD. J Clin Child AdolescPsychol 40: 191-203.
- Brian A, Primack, Kristy M, Hendricks, Meghan R, et al. (2013) Parental Efficacy and Child Behavior in a Community Sample of Children with and without Attention-Deficit Hyperactivity Disorder (ADHD) AttenDeficHyperactDisord4: 189-197.
- Cunningham CE (2007) A family-centered approach to planning and measuring the outcome of interventions for children with attention-deficit/hyperactivity disorder. AmbulPediatr 7: 60-72.
- Johnston C, Ohan JL (2005) The importance of parental attributions in families of children with attention-deficit/hyperactivity and disruptive behavior disorders. Clin Child FamPsychol Rev 8: 167-182.
- Chorpita BF, Daleiden EL (2002) Tripartite dimensions of emotion in a child clinical sample: measurement strategies and implications for clinical utility. J Consult Clin Psychol 70: 1150-1160.
- Stanley P, Stanley L (2005) Prevention through parent training: Making more of a difference. Kairaranga6: 47-54.
- Webster-Stratton C, Reid J, Hammond M (2001) Social skills and problem-solving training for children with early-onset conduct problems: who benefits? J Child Psychol Psychiatry 42: 943-952.
- Jaswinder K, Ghuman L, Eugene Arnoldand Bruno J, Anthony (2008) Psychopharmacological and Other Treatments in Preschool Children with Attention-Deficit/Hyperactivity Disorder: Current Evidence and Practice.J Child AdolescPsychopharmacol 18: 413-447.
- McGoey K, DuPaul G (2000) Token reinforcement and response cost procedures: Reducing the disruptive behavior of preschool children with ADHD.SchPsychol Q 15: 330-343.
- Corrin GE (2003) Group Training versus Parent and Child Group Training for Young Children with ADHD.
- Oortmerssen EE, Vedel E, Koeter MW, de Bruijn K, Dekker JJM, et al. (2013) Investigating the efficacy of integrated cognitive behavioral therapy for adult treatment seeking substance use disorder patients with comorbid ADHD: study protocol of a randomized controlled trial. BMC Psychiatry13: 132.
- Safren SA, Sprich S, Mimiaga MJ, Surman C, Knouse L, et al. (2010) Cognitive behavioral therapy vs relaxation with educational support for medication-treated adults with ADHD and persistent symptoms: a randomized controlled trial. JAMA 304: 875-880.
- Emilsson B, Gudjonsson G, Sigurdsson JF, Baldursson G, Einarsson E, et al. (2011) Cognitive behaviour therapy in medication-treated adults with ADHD and persistent symptoms: a randomized controlled trial. BMC Psychiatry 11: 116.
- Solanto MV, Marks DJ, Wasserstein J, Mitchell K, Abikoff H, et al. (2010) Efficacy of meta-cognitive therapy for adult ADHD. Am J Psychiatry 167: 958-968.
- Shier AC, Reichenbacher T, Ghuman HS, Ghuman JK (2012) Pharmacological Treatment of Attention Deficit Hyperactivity Disorder in Children and Adolescents: Clinical Strategies. J Cent NervSyst Dis 5: 1-17.
- Kraut AA, Langner I, Lindemann C, Banaschewski T, Petermann U, et al. (2013) Comorbidities in ADHD children treated with methylphenidate: a database study BMC Psychiatry 13:11.
Citation: Alamuti E, Mohammadi MR, Borjali A (2016) Comparison of Child and Parent Cognitive Behaviour Therapy on Reduction of Attention Deficit Hyperactivity Disorder Symptoms in Children. J Child Adolesc Behav 4: 285. Doi: 10.4172/2375-4494.1000285
Copyright: © 2016 Alamuti ES, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 11445
- [From(publication date): 4-2016 - Apr 19, 2024]
- Breakdown by view type
- HTML page views: 10633
- PDF downloads: 812